They look natural, feel secure, and restore your smile—but are dental implants really as safe as they seem? Behind the confident grin lies a procedure that involves more than meets the eye. Before you commit to this popular solution for missing teeth, there are essential safety factors you need to understand. Let’s uncover what you might not expect.
TL;DR:
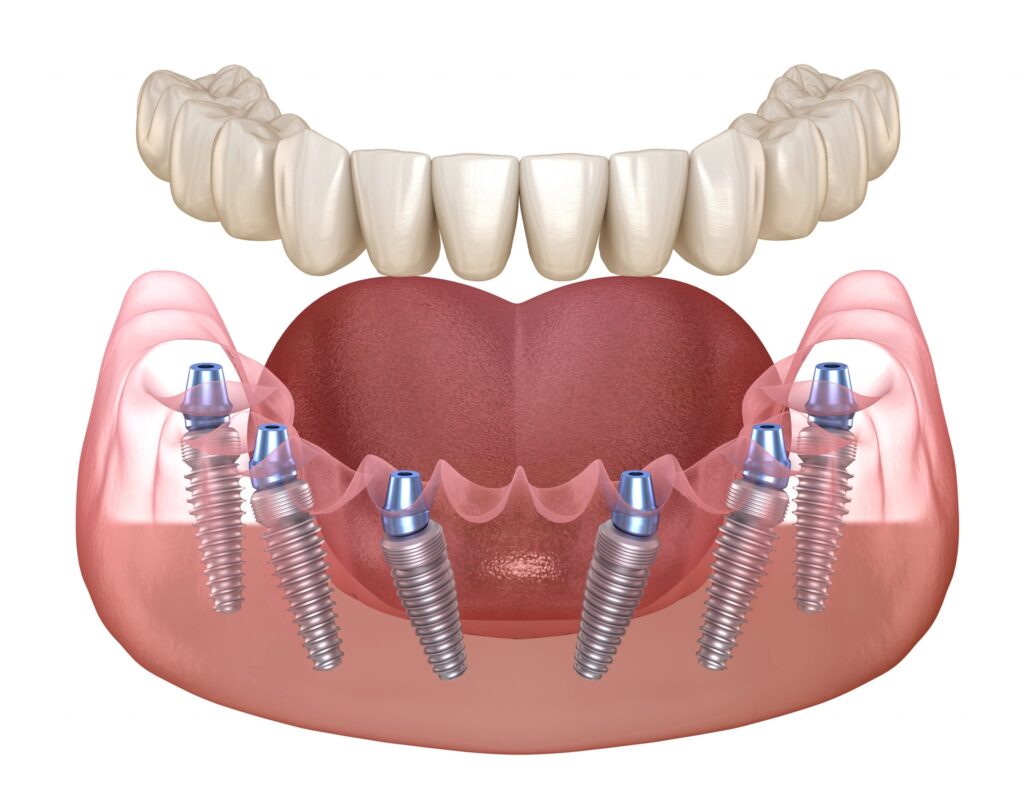
Dental implants are a safe, well-researched tooth replacement option with success rates of 90–98% over 5–15 years when properly placed and maintained. Risks include short-term issues (infection, bleeding, nerve or sinus injury, implant movement) and long-term complications (gum inflammation, peri-implantitis, bone loss, mechanical failures). Risk factors such as smoking, diabetes, poor oral hygiene, and bruxism increase complications. Implants use high-quality, biocompatible materials like titanium and zirconia, with advanced imaging and minimally invasive techniques improving precision and safety. Long-term success depends on excellent oral hygiene and regular professional follow-up.
Need dental implants? Reach out for dental implants Forest Hills, NY 🦷
What Are the Risks of Getting Dental Implants?
Dental implants are generally considered a safe and effective solution for replacing missing teeth, but like any surgical procedure, they carry potential risks. Comprehending both the short- and long-term complications can help patients make informed decisions and take appropriate steps to minimize these risks.
Short-Term Risks
During surgery and the early healing period, patients may experience infection, bleeding, or wound dehiscence—where the surgical site reopens and may require resuturing or antibiotics. There’s also a risk of damage to nearby anatomical structures such as nerves, blood vessels, or sinuses. This can result in numbness, tingling, or sinus complications. Additionally, if the implant moves even slightly before it stabilizes, it may interfere with osseointegration—the essential process where the implant bonds with the bone.
Long-Term Risks
Over time, gum inflammation around the implant may develop. Peri-implant mucositis, a reversible condition, affects up to 50% of patients, while peri-implantitis, a more severe condition involving bone loss, occurs in about 10% of cases. Bone loss around the implant, even without infection, can also threaten the long-term success of the implant. Mechanical complications such as implant fracture, loose screws, or problems with the crown, although less common, can still occur. Rarely, allergic or inflammatory reactions to titanium particles have been reported.
Contributing Risk Factors
Certain factors can increase the likelihood of complications. These include smoking, diabetes, poor oral hygiene, teeth grinding (bruxism), a thin jawbone, and neglecting regular maintenance visits. Managing these factors and following a structured care plan can significantly improve the outcome and longevity of dental implants.
Dental Implants Are Clinically Proven
These implants are not a new or experimental approach—they are a thoroughly researched and well-established treatment option for tooth replacement. Their reliability is backed by decades of scientific evaluation and clinical experience, making them a trusted choice in restorative dentistry.
Numerous long-term studies consistently report success rates of 90–95% over periods ranging from 5 to 15 years. These outcomes highlight the durability and predictability of dental implants when placed and maintained properly. Such high success rates have made implants a standard solution for restoring function and aesthetics.
International consensus organizations, such as the European Federation of Periodontology and the ITI, have developed evidence-based guidelines to prevent complications and enhance outcomes. These protocols stress the importance of individualized planning and careful execution.
High Success Rate in Patients Worldwide
It has been proven to be a reliable solution for tooth replacement across different patient groups and clinical settings. Research consistently shows strong implant survival and patient satisfaction, even in complex cases or with alternative materials.
- Implant Survival Rates: Consistently range from 93–98% over 5–10 years, depending on implant type and the specific restoration used.
- Long-Term Outcomes: A large 10-year retrospective study found 44% of patients had peri-implant mucositis and only 5–6% experienced peri-implantitis, indicating that most implants remain stable over time.
- Material Performance: Alternative materials like zirconia and titanium-zirconium (Ti–Zr) alloys show high survival rates—over 95% within 1–7 years of placement.
- Success with Bone Augmentation: Implant success remains strong even when bone grafting is required, with success rates around 90–95% in pristine sites and slightly lower in grafted areas.
High-Quality, Biocompatible Materials
Dental implants are crafted from materials selected for their exceptional compatibility with the human body and long-term durability. These materials play a essential role in ensuring successful integration with bone and the overall longevity of the implant.
- Titanium: Widely regarded as the industry standard, titanium is corrosion-resistant and forms a stable oxide layer that promotes strong bonding with bone. It also offers excellent resistance to fatigue, making it a durable choice for long-term function.
- Zirconia: As a non-metal alternative, zirconia provides both strength and aesthetic benefits. It resists plaque accumulation and is a suitable option for patients with metal sensitivities or specific cosmetic concerns.
- Advanced Materials and Treatments: Innovations like titanium-zirconium (Ti–Zr) alloys and enhanced surface treatments are improving outcomes further. These advancements support better osseointegration and greater durability, especially in patients with challenging bone conditions.
Minimally Invasive and Controlled Procedure
Modern implant procedures are carefully planned and executed with patient comfort and precision in mind. Advanced imaging technologies like cone-beam computed tomography (CBCT) are used before surgery to evaluate bone volume, locate nerves, and assess sinus proximity. This level of planning allows for highly accurate placement and reduces the risk of complications.
The procedure itself is typically minimally invasive and performed under local anesthesia. Small incisions and sutures are used to limit tissue disruption and support quicker healing. Attention to detail during surgery—such as careful flap management and tension-free closures—helps minimize issues like wound dehiscence and promotes optimal recovery.
Additionally, the use of guided surgery techniques and the expertise of experienced clinicians enhance the precision of implant angulation and positioning. This controlled approach not only improves the overall outcome but also contributes to a more predictable and efficient healing process.
Comprehensive Postoperative Care and Follow-Up
Effective postoperative care is essential to ensure the long-term success of dental implants. Immediately following surgery, patients are advised to manage swelling, avoid hard or chewy foods, and use pain relievers as directed. If prescribed, antibiotics should be taken exactly as instructed to reduce the risk of infection during the healing phase.
Maintaining excellent oral hygiene is equally important. Brushing, flossing, and possibly using antimicrobial mouth rinses help prevent complications. Poor hygiene can lead to peri-implantitis, a serious inflammatory condition that threatens implant stability. Diligent care at home plays an essential role in preserving the health of the surrounding tissues.
Ongoing follow-up is just as vital. Regular dental checkups allow for early detection of problems like mucositis or mechanical wear. Scheduled maintenance visits have been shown to reduce the risk of peri-implantitis by up to tenfold.
Sources.
Ozkan, A., Çakır, D. A., Tezel, H., Sanajou, S., Yirun, A., Baydar, T., & Erkekoglu, P. (2023). Dental implants and implant coatings: A focus on their toxicity and safety. Journal of Environmental Pathology, Toxicology and Oncology, 42(2).
Sun, T. M., Lan, T. H., Pan, C. Y., & Lee, H. E. (2018). Dental implant navigation system guide the surgery future. The Kaohsiung journal of medical sciences, 34(1), 56-64.
Panchal, M., Khare, S., Khamkar, P., & Bhole, K. S. (2022). Dental implants: A review of types, design analysis, materials, additive manufacturing methods, and future scope. Materials today: proceedings, 68, 1860-1867.
Key Takeaways:
General Safety
- Dental implants are a well-established, safe, and effective tooth replacement option with long-term success rates of 90–98% when properly placed and maintained.
Short-Term Risks
- Possible issues include infection, bleeding, wound reopening, nerve/blood vessel/sinus damage, numbness, or implant movement affecting bone integration.
Long-Term Risks
- Gum inflammation (peri-implant mucositis) in up to 50% of patients; peri-implantitis with bone loss in about 10%.
- Other risks: bone loss without infection, implant/crown fractures, loose screws, and rare allergic reactions to titanium.
Risk Factors
- Smoking, diabetes, poor oral hygiene, bruxism, thin jawbone, and skipping maintenance visits increase complication likelihood.
Clinical Evidence
- Backed by decades of research and global guidelines from organizations like EFP and ITI emphasizing individualized planning.
- Strong survival rates across patient groups, including cases with bone grafting or alternative materials (zirconia, Ti–Zr alloys).
Material Quality
- Titanium: durable, corrosion-resistant, bonds well with bone.
- Zirconia: strong, aesthetic, resists plaque, suitable for metal sensitivity.
- Advanced alloys and surface treatments improve durability and integration.
Procedure Precision
- Advanced imaging (CBCT) and guided surgery ensure accurate placement and reduce complications.
- Minimally invasive techniques with careful surgical management support faster healing.
Postoperative Care
- Essential to follow instructions for swelling control, diet, medication, and oral hygiene.
- Regular dental checkups and maintenance visits significantly reduce risks, especially for peri-implantitis.